Learn About Asthma - Canadian Children's Asthma Society Website
Main menu:
Learn About Asthma
Young Children And Asthma
How Is Asthma Diagnosed?
Asthma is hard to diagnose in very young children as there is no actual test that could be performed. Instead the doctor relies on the information given to them by the parent on the child’s breathing and any issues with the respiratory system such as shortness of breath. Thus, Asthma is mainly diagnosed on the child’s history, the pattern of symptoms, and the family’s medical history.
Some family doctors may prescribe Asthma medications for a trial period to see if the child’s breathing improves. It is much easier to diagnose Asthma with older children that are able to communicate directly with the doctor.

Could Your Child Have Asthma?
It is common for a child that has Asthma to develop symptoms in their first year in life and be diagnosed with Asthma. Asthma is more common in children who have parents or other siblings in the family that have Asthma. Although it is not necessarily a hereditary disease, the family in household experience and are exposed to the same environmental surrounding that could cause Asthmatic symptoms. For example, a family residing in an industrial city will be exposed to more severe carbon based particles in the air than a family living in the suburbs. Also, family units that have allergies or allergic skin problem such as eczema are more prone to having Asthma.
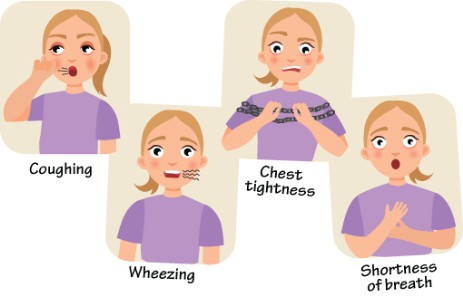
If the child has symptoms such as a chronic or long lasting cough, trouble breathing or wheezing, they could have Asthma. These symptoms may occur in conjunction with colds or chest infections. Also, colds that do not seem to go away, may actually be Asthma. It is always best to consult a doctor and have the child assessed for Asthma.

What To Do If Your Child Has Asthma
If your child has been diagnosed with Asthma by a doctor, then there are some very important steps that must be made:
Identify the child’s triggers and avoid them as much as possible.
Learn about the child’s Asthma medications that have prescribed by the doctor. Know how to administrate them correctly and exactly what they are used for (Controller or Reliever).
Make regular visits with your doctor to keep informed and to help control the child’s Asthma.
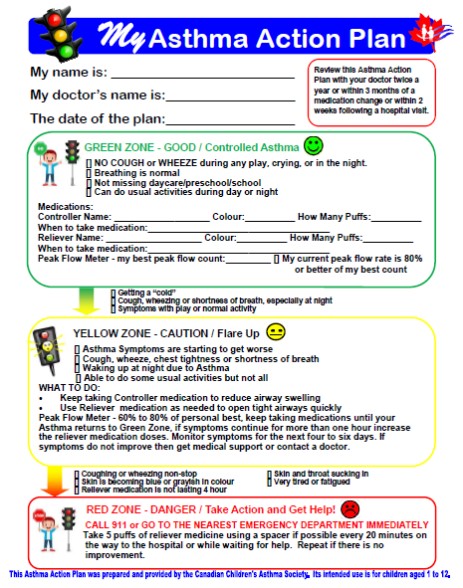
Develop an Asthma Action Plan with your doctor in a written format. You may download a template for the Asthma Action Plan from our website at the bottom of this information. As soon as you notice any Asthma issues, check your plan for any changes in treatment.
An Asthma Diary or Journal to keep track of changes in the child’s Asthma is also a great idea.
Your doctor may refer the child to see a Respiratory Therapist to learn more about Asthma or an Allergist to conduct allergy tests.
Learn as much about Asthma. Ask about our next community Asthma education clinic.
Know Your Child’s Asthma Triggers
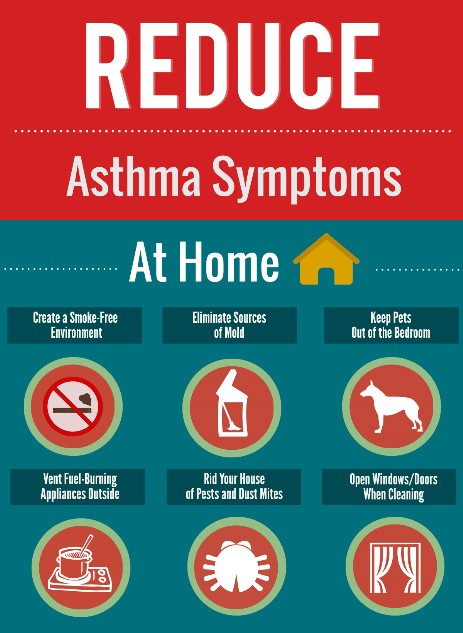
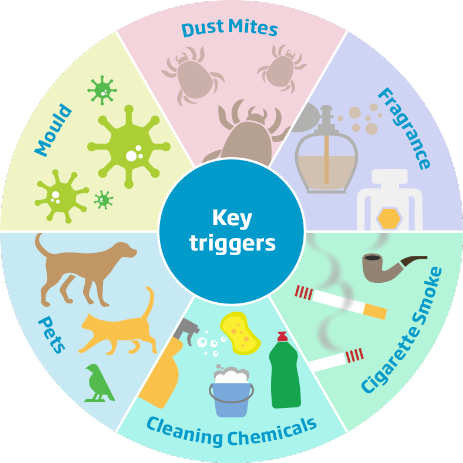
A trigger is anything that makes Asthma worse and may lead to an Asthma attack. The most common Asthma triggers for children under the age of four are colds and tobacco smoke. However, any other environmental surroundings in the home could effect a very young child or infant which include animal dander, house mold, home dust mites, an unclean home environment, plants within the household, and exposure to house cleaning products.
Even after a cold has settled, the Asthma symptoms and swelling in the airways could last for many weeks. Young children that are exposed to second hand smoke from either tobacco or cannabis could develop severe respiratory problems which could lead to the development of Asthma. The younger the child is and the exposure of second hand smoke make the respiratory and Asthma issues extreme and the child may come down with more colds as their immune system could be compromised.
For health and safety of your child, it is always best to try to limit and if possible eliminate the child to exposure of these home elements mentioned above that trigger Asthma or may cause severe respiratory difficulties.
Signs Of Worsening Asthma
Seeing the warning signs of worsening asthma will greatly help being proactive in preventing an Asthma attack. Watch for these signs:
The child gets a cold
Coughing or wheezing during sleep or upon the child waking up
Coughing or wheezing with activity, laughing or crying
Decreased energy levels
Needing Reliever medicine more than once a day or three times a week for symptoms.
Early warning signs let the you, the parent, know that problems are starting. When you see any early warning signs, follow your Asthma Action Plan. Download a template for your child’s Asthma Action Plan on this website at the bottom of all the information. The plan should be prepared in conjunction with your doctor.

Managing An Asthma Attack
Signs Of An Asthma Attack
If your child has been diagnosed with Asthma, there are four early signs of Asthma getting worse:
1) The child has the start of a cold or runny nose.
2) The child is coughing at night time or in the early morning.
3) You are able to hear wheezing (whistling noises) coming from the child. This would indicate that there is a shortness of breath or chest tightness.
4) If the child uses the Reliever medication much more than prescribed by the doctor or the Reliever medication is not lasting as long.
The signs of an Asthma attack getting much worse include:
1) If the child feels short of breath and complains of a tight feeling in their chest, it may be start of a severe Asthma attack. The child may have trouble exercising, talking or even eating when this occurs.
2) The child’s wheezing is much more noticeable as the child struggles more to breath. During a severe Asthma attack, there may be little or no noise because the airway passages are very much blocked.
3) When the child breathes in, the skin may be sucked in at the throat, collarbone, or between or under the ribs.
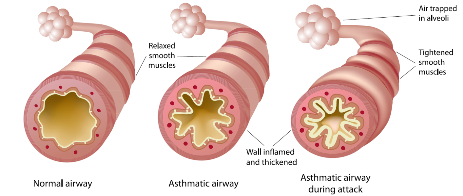
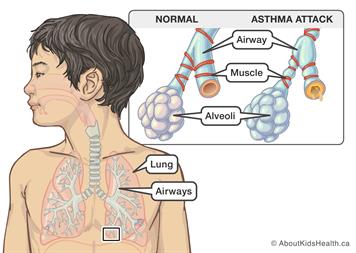
What Happens During An Asthma Attack
A normal airway has a good airway passage flow that is clearly open and the outer muscles are relaxed and smooth. During an Asthma attack, the inside of the airway passages become swollen and mucous is created. The muscles around the outside of the airways tighten and decrease the flow of air flow. The walls of the airway become inflamed and thickened. When the opening inside the airways becomes smaller, it becomes harder to breathe.
What To Do If A Child Is Having An Asthma Attack
It is always very important to STAY CALM and never to panic if a child is having an Asthma attack. Panicking may cause the child to feel much more stressed and anxious which may worsen the situation.
The first thing needed is to identify the child’s Asthma triggers and then move the child away from them. Secondly, help administer the Reliever medication for the current symptoms. The medicine should help the child within ten minutes as it helps open the airways in the lungs. Allow the child to have the Reliever medicine more times if the chest becomes tight or the breathing becomes worse again. If the Reliever medicine is not working as well or is required often during the day (more than once every four hours), then contact a doctor. After the Reliever medicine is given, help the child to relax.
When It Is Time To Go To The Hospital’s Emergency
If the child needs their Reliever medicine quite often in a short period of time (more than two puffs in a three hour time span) and the Asthma attack has not come under control or the Reliever medicine has not helped improve the child’s breathing within ten minutes of their first use then GO TO THE NEAREST EMERGECY!
The child may use the Reliever medicine as much as needed on the way to the Hospital Emergency Department.
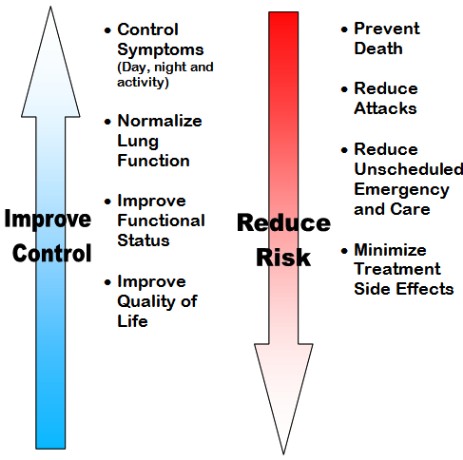
Ways To Prevent An Asthma Attack
The parents or guardians of the child should always take an active part in caring for the child that has Asthma. Always watch for signs that Asthma is getting worse. Work on an Asthma Action Plan with the child’s doctor and know and understand how to use it. An Asthma Action Plan is a personalized program for managing the child’s Asthma. The plan is used as strategy in identifying triggers that cause the child’s Asthma to flare up. The plan helps in managing triggers and steps to take when the Asthma gets out of control. Knowing the child’s Asthma triggers are very important. Learn about the different Asthma medications the child needs to properly manage their Asthma. It is always a good idea to review the Asthma Action plan with the child’s doctor a couple of times per year. With proper management, Asthma could be controlled.

Controlling Asthma
The Goal Of Asthma Control
If the child is using and needs their Reliever medicine more than once a day or three to four times a week for their Asthma symptoms, then their Asthma control is poor and they are at a risk for an Asthma flare-
Having good Asthma Control allows the child to have:
Normal Activities
Normal Sleep
No missed school time
No issues with Asthma symptoms during the day
No need for their Reliever medicine beyond what is prescribed by their doctor
No visits to the hospital emergency from their Asthma symptoms or flare-
ups.
Asthma Can Be Controlled
Children with Asthma should be able to lead normal lives. Keeping the child’s asthma under control is very important at all times. By keeping the child’s Asthma under control, all children with Asthma should be able to be active without Asthma problems which include flare-
Work together with your child’s doctor and/or Asthma Educator to control the child’s Asthma. Always keep learning as much as you could about Asthma.
Asthma Management is about having the ability to create a plan of action that will help control your child’s Asthma. If the Asthma Action Plan is successful, then control should be improved and the risk factors are reduced.
Why Is Asthma Control Important
Children with good Asthma control can take part in normal childhood activities and participate better in school. When Asthma is under control, children also have much fewer and less severe Asthma flare-
Know what the child’s Asthma medicines do and learn how to use them properly.
Ask the child’s doctor to help with an Asthma Action Plan. See the doctor twice a year, every six months to review the plan.
Know the signs of the child’s Asthma becoming worse.
Know the child’s Asthma triggers and to stay away from them.
Asthma Medications & Devices
What Should Be Known About Asthma Medications
Why it is used?
How it works?
How to use it?
How often and long it should be used
Is there any side-
effects from the medications or problems if taken with other medications? What are the financial costs?
Asthma Medications & Devices
There are a number of different medications for the treatment of Asthma, however most of them do the same two things: 1) help relieve symptoms immediately in the short term and help prevent an Asthma flare-
It is very important that the child who has Asthma always has access to their medications, especially their reliever medicine to help prevent an Asthma flare-
If the reliever medication is used often and more than prescribed, it is then important to consult the family doctor or a respiratory specialist as the medication may not be working properly and the Asthma may be out of control.
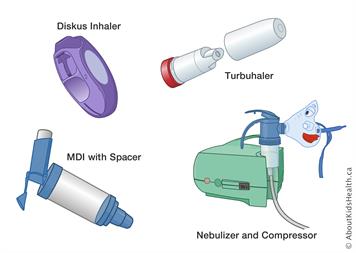
Asthma medications come in a few different forms that include aerosols, vapes, powders, tablet and liquids. Most Diskus inhalers and Turbuhalers are filled with powder forms. Nebulizers give off the medication in a vapor form as most come in a puffer which are liquids and once sprayed they are spread as aerosols.
There are many kinds of devices used but the most common is a spacer which us used with the puffer to help get the correct dosage of medication to the child. Other devices include compressors, dosage readers and respiratory meters.

Kinds of Medications Used To Treat Asthma
Two main kinds of Asthma medicines exist:
Controllers
Relievers
Controllers work to help prevent swelling and extra mucous buildup inside the airways over a period of time.
Relievers relax the outer muscles on the outside of the airways. Some of the reliever medicines are referred to as bronchodilators as they usually act fast when Asthma symptoms arise.
The majority of Asthma medications are inhaled into the lungs in the form of powders, mists and vapours. However there is also digestible tablets that could be taken which are usually controller medicines for long term use.
Depending on the severity and the control of Asthma symptoms, not every child will need to have both medications. More serious Asthma cases will require both medications to be used. However, every child that has been diagnosed with Asthma should have access to a reliever medicine.
Reliever Medications
Reliever medications are meant to be used when the signs of Asthma symptoms arise and to help prevent a major Asthma flare-
Relievers are meant to be used as short term medicine that acts fast and for a short period of time to get the Asthma under control.
Relievers could be administered ten to fifteen minutes prior to any exercise or physical exertion to help prevent Asthma symptoms.
Reliever usually act within ten minutes to relieve Asthma symptoms.
If the reliever medicines is required more than three or four times a week, this is a major sign that Asthma is out of control.
The most common type of reliever medicine is Salbutamol which usually comes in a light blue inhaler. Other reliever medicines include Terbutaline and Formoterol.
Controller Medications
Controller medications work over a period of time and are used as a long term medication in treating Asthma and are also known as Preventers. These kinds of medications are very important to those who have Asthma in controlling their symptoms.
There are number of different kinds of controller medicines that may or may not have a steroid component to them. Some of the medications may be increased if Asthma symptoms get worse. Some of the medications come in vapour or liquid form, as others may come in a powder or pill form. An example of a pill form is Monteukast or better known by its trade name Singular. Fluticasone or FloVent comes in a liquid form and is inhaler with the use of a puffer which gives off a mist of the medication.
Combination Medications
Combination medications are mixtures of various medicines that contain both a Controller part and a Reliever medicine for long-
It is always very important to consult a doctor before using any medications and only use medications that are prescribed for the child. Some of the medications may have proper dosages for children as Adult medications may contain a higher dosage which could lead to other issues if a child takes it. Never use expired medications or any medications in a defective holder or device.
Samples of Reliever Medications
Samples of Controller Medications
Allergies & Asthma
What Is An Allergy?
An allergy is a sever reaction to something that the body can not tolerate. A sever allergy reaction is also know as a Anaphylaxis. Depending on the allergic reaction, different parts of the child’s body could be affected or the allergic reaction may affect the entire body system. When this occurs, the allergy reaction is much more severe and emergency medication attention is needed. This is also know as Anaphylaxis shock when either the entire body of the child or vital organs are affected. One reaction may compound on another. For example, issues with respiration may lead to increased blood pressure which could lead to fainting or even cardiac arrest.
Allergies may be developed over time with an extended exposure or a child could be naturally born with certain allergies.
Allergies that are developed over time are usually caused by industrial or commercial toxins. As natural allergies are usually caused by digested foods such as peanut butter or seafood, and natural exposures to environment such as dogs, cats or bees.
The reactions could be unpredictable in some cases and occur within a short period of time after contact with the substance or trigger is made.
Children that have Asthma and allergies may have two or more medications to deal with symptoms and reactions.
Antihistamine medications will not prevent or stop anaphylaxis or help with an Asthmatic episode.
Keep in mind that a sever allergic reactions, especially with a child that also has Asthma is a medical emergency that could be fatal if not treated correctly and quickly.

Common Signs Of An Allergy
There are many reactions to the various allergies that may occur in children and not all children will experience the same reactions. If a child has allergies from a scent toxin formed by either naturally or commercial chemical, that child may either have an Asthma episode as another child may experience fainting or dizziness with no respiratory complications.
Some of the most common allergy reactions in children include:
Itching in a specific area or throughout the entire body
Hives may develop and could become severe
Swelling of the face, lips, tongue or throat may occur either suddenly or over a short period of time depending on the exposure that caused the allergy reaction
Severe drooling or trouble swallowing
Vomiting
Breathing problems including cough, wheeze or being short of breath
What Is The Connection Between Allergies & Asthma
Allergic reactions could become worse if the child also has Asthma. It could be much worse if the Asthma is not in control. Having issues with breathing may occur with either Asthma or from an allergic reaction. However the medications used to treat the breathing issues will vary depending on what the cause or trigger is. Breathing issues are usually more brought on faster when the cause is an allergic reaction.
Asthma medications, such as inhalers, will not work for an allergic reaction. Instead the medication needed is an Adrenalin which is also known as epinephrine.
Some of the allergies a child may have, could cause Asthma related breathing issues that could be treated by an Asthma medication. For example, dog or cat dander may trigger Asthma symptoms and could be treated for breathing related issues with the Asthma medication, but the medication will not help decrease the allergic reaction. Some allergic reactions may not trigger breathing problems that would lead to Asthma symptoms, but will cause other effects such as itching or swelling.
How To Use The Epinephrine Auto-
A common name for the device is an EpiPen. To administrate the medication, first hold the device in your fist, remove the cap off, and then place the tip against the mid outer thigh and push against the leg firmly and quickly until you hear a click sound. Hold the device in place for 5 seconds as the medication is being administered. Remove the device and get help or transport the child to the nearest hospital.
Managing Allergies
There are a number of different kinds of allergies. The most common include:
Natural Environmental
Commercial Chemical
Food
Viral or Bacterial
Depending on the kind of allergy a child may have, treatments will be different. Some may include medications as others may require more simpler treatments such as natural remedies or rest. It is always best to consult a family doctor or an Allergist to confirm what allergies the child may have.
It is best to always try to avoid the things that the child is allergic to. If the child requires medication such as an EpiPen to treat the allergy reaction, then it is always best to have the medication available for the child in case of an emergency. If medication is used, always check the expiry dates as expired medication may not be effective and may cause other side effects. Having the right medicine and at the right time may save the life of the child. Learn and understand how to administrate the medication and also the volume or amount that needs to be given. Too little may not be effective as too much medication may lead to an overdose. If the allergic reaction does not subside or reduce within a reasonable amount of time, then emergency services should be alerted by calling 911 or if a hospital is near by then the child should be taken to the Emergency Department.
If the allergy trigger is air born, such as scents, it may be a good idea to have an air purifier in the child’s bedroom at their home.
Make sure to always inform those who care for the child about the allergies. Notify teachers, caregivers, family and friends. If medication is used, then explain how to use the medication to those involved. Any child that has a severe allergy should also wear a Medical Alert bracelet.

Going On A Vacation?
How To Cope With A Child's Asthma
How To Get Ready For A Vacation
Travelling is ok with children that have Asthma. Asthma shouldn’t stop any child from going on a vacation, camping, a sleepover, or even a school trip to an event or place.
Planning ahead is a major key factor in ensuring a relaxing and enjoyable vacation. You need to understand the environment of where you will be going to vacation and the changes that could occur in that environment that may effect the breathing of the child and their ability to control their asthma. It is important to know the child’s Asthma triggers and if they will be present at the location of the vacation that you will be going to.
Make sure that your child’s asthma is under control before going on a vacation. Following your child’s Asthma Action Plan is very important. Talk to your doctor before going on vacation and update the Asthma Action Plan if needed. Make sure your child’s Asthma medications are up to date (not expired) and are the correct medications being used that the doctor has prescribed according to the current Asthma Action Plan.
What Goes In An Asthma Travel Pack?
Make sure the child’s medications are up to date and not expired. The medication should be clearly labeled with the name of the medication and the child’s name. If a child uses a spacer, make sure it is clean. These are very important items to bring. It is also a great idea to have extra medication or to carry a copy of the prescription in case of loss or the packed medication becomes damaged during the trip.
Contact information is very important. Always bring a list of all the child’s contact information along with the child’s Asthma Action Plan. It is very important to follow the Plan, even being on vacation. A Peak flow meter is another good item to bring along to monitor the child’s breathing.
Quick Relief & Controller Medication
A Nebulizer, Long Term Care Medication & Spacer
Asthma Action Plan
Written Prescription
Health Insurance Card
Child’s Contact Information (Healthcare provider contact information)
Prescribed Allergy Medications
Peak Flow Meter

While On Vacation, Things To Do
Always keep the child’s Asthma medication available and ready when travelling instead of packing it away in a luggage.
Always use the Asthma medications at the same time according to the Asthma Action Plan for the child while travelling and while on vacation.
When on vacation, it is very important to know where the nearest hospital emergency is located and also the time it will take to get there.
It is also important to educate and inform the other people who may be with your child of their Asthma and how to treat any Asthma symptoms or flare ups.
Be aware of changing weather patterns during your vacation. Variations in pollen and air pollution in the different area of travel could cause breathing issues. It is best to try to avoid any travel during times where air pollution or pollen is at its highest levels.
If the child's asthma is well controlled, you should be able to enjoy sightseeing, hiking, and other fun activities. Just keep the asthma triggers in mind when planning what you'll do. For example, avoid lots of walking or hiking when air pollution or pollen counts are high or in very cold and dry weather. If you're camping, keep your child away from campfires. Ski vacations or hiking trips aren't out of the question. But make sure you plan for plenty of rest (indoors if possible), and carry your child's quick-
Be prepared to change your plans if your child is struggling with asthma symptoms.
How Can We Avoid Asthma Triggers During Travel?
It is always a good idea to stay in hotel or motel rooms that are smoke free and are also away from any rooms or areas that allow smoking.
If the child has allergies to pollen or mold, using the air conditioning systems in hotel/motel rooms and in the vehicle is much better than keeping any windows open that may allow pollen to enter. Indoor swimming pools may also contribute to mold, it is best to stay at hotel that does not have an indoor pool or at least in a room which is a fare distance from any indoor pools.
If the child has allergies towards pet dander or fur, it is also best to stay in a pet free hotel/motel.
If you are going somewhere with the child that is new, be aware of possible new triggers that the child may come in contact with.
Can Children With Asthma Travel Alone?
If the child travels solo (to sleepover camp, to friends or family, etc.), talk with the adults in charge. It's very important for parents, counselors, or chaperones to have copies of the asthma action plan, a list of medicines, and all emergency phone numbers. Also send written (and notarized) permission for them to care for your child in an emergency.
Sit down with your child before the trip to go over the asthma action plan and what to do in an emergency. Your child should know his or her asthma triggers, when and how to take medicines, and how to recognize the signs of a flare-
Physical Fitness / Healthy Lifestyle And Asthma
Living A Healthy Lifestyle With Asthma
Children with Asthma can lead a healthy active lives. Asthma can be different for each child and unfortunately at this time it cannot be cured, but it can be controlled by living a healthy lifestyle and proper Asthma medication use.
Healthy eating will help children with Asthma. Fresh fruit and vegetables are full of antioxidants, which may improve lung health which helps in avoid asthma attacks. Eating fish often may also help with asthma. Eating too much saturated fat may prevent Asthma medicines working properly. Limit the amount of convenience foods high in saturated fat, and choose lean meats, skinless chicken and reduced-
Enjoy a physically active lifestyle. Getting more active can make a child feel better. Don’t let Asthma stop a child from being physically active. Choose an activity the child enjoys, as this can help motivate them, and aim for at least 30 minutes of moderately intense physical activity every day or most days. Moderately intense physical activity means any activity that makes the child breathe noticeably faster and deeper than usual, but does not make them puff and pant. Asthma symptoms after physical activity are common but treatable, so don’t let this put a child off being active. If being physically active causes asthma symptoms, tell the doctor so a treatment that works best can be used. This could be as simple as taking extra puffs of the reliever before the warm up. Consider getting the child involved in structured exercise training, as people with asthma who participate in this sort of training may feel better.

Physical Fitness And Asthma
Many people may ask “Why exercise is good for children with Asthma?” Positive physical fitness including exercising and participates in various physical sports improves the way lungs work. Staying active is very important to keep lungs healthy and working properly. Physical fitness also boosts the immune system by causing more active respiratory air circulation and blood circulation which oxygenates the body, thus keeping it clean from infections and viruses.
Physical Fitness also helps keep weight down in children. Having a healthy weight makes it easier to breathe. Physical fitness also makes the child feel better and more positive about their abilities thus keeps them in a good mood.
Getting into a regular exercise routine or participating in an active sport is a great idea for everyone, especially for children who are growing. Children that have Asthma should be able to participate in almost any exercise, sport or play. Did you know that One in every ten Olympic athletes have Asthma? All those athletes where children at some time.
Well controlled Asthma should not limit exercise, however exercise may trigger Asthma symptoms soon after the child may start. If Asthma stops the child from being active, then their Asthma is out of control and the child needs to see a doctor.
There is a few activities that are not recommended for people that have Asthma. They include any activities with high air pressure or activities that may put severe strain on the lungs of children. These activities include scuba diving and sky diving.

Asthma Symptoms During Physical Fitness
It is best to not start exercising if you have any Asthma symptoms. Asthma symptoms may include coughing, wheezing, shortness of breathe or a tight feeling in the chest. Other symptoms may also include tiring easily or not being able to perform effectively during exercise or any sports activity.
Prolonged physical activities such as running, soccer, or basketball is more likely to cause symptoms than short bursts of activities such as volleyball, bowling, golfing or tennis.
It is best to exercise in a warm, humid setting as it may be less likely to cause symptoms.
Remember, if a child has Asthma, physical activities and fitness could cause symptoms, but the physical activity or fitness does not cause Asthma.

How To Prevent Asthma Symptoms
The best way to prevent Asthma symptoms is by keeping Asthma under control. It is always best to warm up before exercising or any physical activity and cool down afterwards.
If necessary, use the Asthma Reliever medication ten to fifteen minutes before any physical fitness or activity. If the Reliever medication is used more than it is prescribed by the doctor, then the Asthma may be out of control and it best to consult the doctor.
If possible, the child should breathe through their nose, instead of their mouth when involved in any physical activity.
When air pollution is bad or pollen counts are high, it best for the child to avoid doing any physical activities outdoor. If possible exercise or play indoors.
If playing outside in very cold air, it is recommended to cover the child’s mouth or nose with a face covering such as a scarf.

To receive a PDF copy of the Children's Asthma Action Plan Form,
please email us at CanadianChildrensAsthma@gmail.com